Derek Thompson
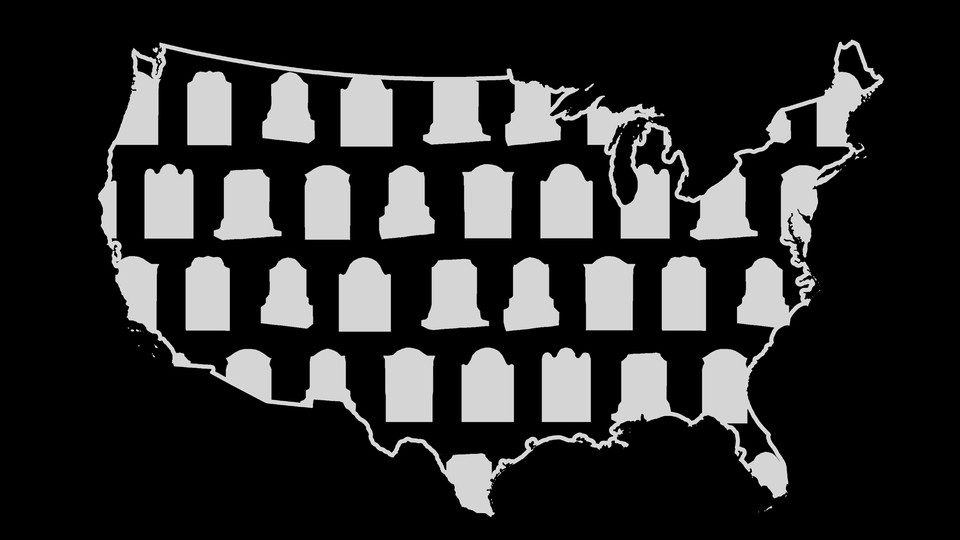
America has a death problem.
 No, I’m not just talking about the past year and a half, during which COVID-19 deaths per capita in the United States outpaced those in similarly rich countries, such as Canada, Japan, and France. And I’m not just talking about the past decade, during which drug overdoses skyrocketed in the U.S., creating a social epidemic of what are often called “deaths of despair.”
No, I’m not just talking about the past year and a half, during which COVID-19 deaths per capita in the United States outpaced those in similarly rich countries, such as Canada, Japan, and France. And I’m not just talking about the past decade, during which drug overdoses skyrocketed in the U.S., creating a social epidemic of what are often called “deaths of despair.”I’m talking about the past 30 years. Before the 1990s, average life expectancy in the U.S. was not much different than it was in Germany, the United Kingdom, or France. But since the 1990s, American life spans started falling significantly behind those in similarly wealthy European countries.
According to a new working paper released by the National Bureau of Economic Research, Americans now die earlier than their European counterparts, no matter what age you’re looking at. Compared with Europeans, American babies are more likely to die before they turn 5, American teens are more likely to die before they turn 20, and American adults are more likely to die before they turn 65. At every age, living in the United States carries a higher risk of mortality. This is America’s unsung death penalty, and it adds up. Average life expectancy surged above 80 years old in just about every Western European country in the 2010s, including Portugal, Spain, France, Italy, Germany, the U.K., Denmark, and Switzerland. In the U.S., by contrast, the average life span has never exceeded 79—and now it’s just taken a historic tumble.
Why is the U.S. so much worse than other developed countries at performing the most basic function of civilization: keeping people alive?
“Europe has better life outcomes than the United States across the board, for white and Black people, in high-poverty areas and low-poverty areas,” Hannes Schwandt, a Northwestern University professor who co-wrote the paper, told me. “It’s important that we collect this data, so that people can ask the right questions, but the data alone does not tell us what the cause of this longevity gap is.”
Finding a straightforward explanation is hard, because there are so many differences between life in the U.S. and Europe. Americans are more likely to kill one another with guns, in large part because Americans have more guns than residents of other countries do. Americans die more from car accidents, not because our fatality rate per mile driven is unusually high but because we simply drive so much more than people in other countries. Americans also have higher rates of death from infectious disease and pregnancy complications. But what has that got to do with guns, or commuting?
By collecting data on American life spans by ethnicity and by income at the county level—and by comparing them with those of European countries, locality by locality—Schwandt and the other researchers made three important findings.
First, Europe’s mortality rates are shockingly similar between rich and poor communities. Residents of the poorest parts of France live about as long as people in the rich areas around Paris do. “Health improvements among infants, children, and youth have been disseminated within European countries in a way that includes even the poorest areas,” the paper’s authors write.
But in the U.S., which has the highest poverty and inequality of just about any country in the Organization for Economic Cooperation and Development, where you live is much more likely to determine when you’ll die. Infants in the U.S. are considerably more likely to die in the poorest counties than in the richest counties, and this is true for both Black and white babies. Black teenagers in the poorest U.S. areas are roughly twice as likely to die before they turn 20, compared with those in the richest U.S. counties. In Europe, by contrast, the mortality rate for teenagers in the richest and poorest areas is exactly the same—12 deaths per 100,000. In America, the problem is not just that poverty is higher; it’s that the effect of poverty on longevity is greater too.
Second, even rich Europeans are outliving rich Americans. “There is an American view that egalitarian societies have more equality, but it’s all one big mediocre middle, whereas the best outcomes in the U.S. are the best outcomes in the world,” Schwandt said. But this just doesn’t seem to be the case for longevity. White Americans living in the richest 5 percent of counties still die earlier than Europeans in similarly low-poverty areas; life spans for Black Americans were shorter still. (The study did not examine other American racial groups.) “It says something negative about the overall health system of the United States that even after we grouped counties by poverty and looked at the richest 10th percentile, and even the richest fifth percentile, we still saw this longevity gap between Americans and Europeans,” he added. In fact, Europeans in extremely impoverished areas seem to live longer than Black or white Americans in the richest 10 percent of counties.
Third, Americans have a lot to learn about a surprising success story in U.S. longevity. In the three decades before COVID-19, average life spans for Black Americans surged, in rich and poor areas and across all ages. As a result, the Black-white life-expectancy gap decreased by almost half, from seven years to 3.6 years. “This is a really important story that we ought to move to the forefront of public debate,” Schwandt said. “What happened here? And how do we continue this improvement and learn from it?”
One explanation begins with science and technology. Researchers found that nothing played bigger roles in reducing mortality than improvements in treating cardiovascular disease and cancer. New drugs and therapies for high cholesterol, high blood pressure, and various treatable cancers are adding years or decades to the lives of millions of Americans of all ethnicities.
Policy also plays a starring role. Schwandt credits the Medicaid expansion in the 1990s, which covered pregnant women and children and likely improved Black Americans’ access to medical treatments. He cites the expansion of the earned-income tax credit and other financial assistance, which have gradually reduced poverty. He also points to reductions in air pollution. “Black Americans have been more likely than white Americans to live in more-polluted areas,” he said. But air pollution has declined more than 70 percent since the 1970s, according to the EPA, and most of that decline happened during the 30-year period of this mortality research.
Other factors that have reduced the Black-white life-expectancy gap include the increase in deaths of despair, which disproportionately kill white Americans, and—up until 2018—a decline in homicides, which disproportionately kill Black Americans. (The recent rise in homicides, along with the disproportionate number of nonwhite Americans who have died of COVID-19, will likely reduce Black life spans.)
Even then, Black infants in high-poverty U.S. counties are three times more likely to die before the age of 5 than white infants in low-poverty counties. But Schwandt insists that highlighting our progress is important in helping us solve the larger American death problem. “We are wired to care more about bad news than about good news,” he said. “When life expectancy rises slightly, nobody cares. But when life expectancy declines, suddenly we’re up in arms. I think that’s a tragedy, because to improve the health and well-being of our populations, and especially of our disadvantaged populations, we have to give attention to positive achievements so that we can learn from them.”
We’re a long way from a complete understanding of the American mortality penalty. But these three facts—the superior outcomes of European countries with lower poverty and universal insurance, the equality of European life spans between rich and poor areas, and the decline of the Black-white longevity gap in America coinciding with greater insurance protection and anti-poverty spending—all point to the same conclusion: Our lives and our life spans are more interconnected than you might think.
For decades, U.S. politicians on the right have resisted calls for income redistribution and universal insurance under the theory that inequality was a fair price to pay for freedom. But now we know that the price of inequality is paid in early death—for Americans of all races, ages, and income levels. With or without a pandemic, when it comes to keeping Americans alive, we really are all in this together.
No comments:
Post a Comment