Ewen Callaway & Heidi Ledford

People await coronavirus vaccines at a hospital in Glasgow, UK.Credit: Jeff J. Mitchell/Getty
As evidence grows that new variants of the SARS-CoV-2 coronavirus can evade immunity produced by vaccines or previous infections, scientists are exploring the idea of redesigning the vaccines currently being rolled out worldwide.
Researchers are still debating whether the new variants could undercut the effectiveness of these first-generation COVID-19 vaccines. But some vaccine developers are charging forward with plans to update their shots so that they could better target the emerging variants, such as those identified in South Africa and Brazil. These lineages carry mutations that seem to dampen the effects of antibodies crucial to fending off infection. Researchers are also considering the possibility that vaccines against the coronavirus might have to be updated periodically, as they are for influenza.
The best and most immediate way to combat the threat of emerging variants is still probably to quickly vaccinate as many people as possible with current shots, says Mani Foroohar, a biotechnology analyst at the investment bank SVB Leerink in Boston, Massachusetts: “We need to get vaccines in arms and to smother this virus before it blows up in our face again.”
But Foroohar and others expect that, in the future, a bevy of new vaccines will emerge to tackle the COVID-19 variants head on. Nature explores the open questions about updating the world’s coronavirus vaccines.
Will we need updated COVID-19 vaccines?
“I think it’s starting to look that way,” says Kanta Subbarao, a virologist at the Peter Doherty Institute for Infection and Immunity in Melbourne, Australia.
Laboratories worldwide are racing to understand the threat that emerging coronavirus variants pose for vaccines. But early insights from these studies are mixed and incomplete. A variant identified in late 2020 in South Africa, called 501Y.V2 (also known as variant B.1.351), is among the most worrying. Lab assays have found that it carries mutations that sap the potency of virus-inactivating ‘neutralizing antibodies’ that were made by people who received either the Pfizer or Moderna RNA vaccines.
Whether these changes are enough to lower the effectiveness of those vaccines is not clear, says Subbarao. “That is the million-dollar question, because we don’t know how much antibody you need.” Other immune responses that vaccines prompt might help to protect against the effects of variants.
But on 28 January, biotech firm Novavax released data from clinical trials showing that its experimental vaccine, designed to combat the original virus, was about 85% effective against a variant identified in the United Kingdom — but less than 50% effective against 501Y.V2. That drop is concerning, say researchers, because it indicates that 501Y.V2 and other variants like it can cause a significant drop in vaccines’ effectiveness.
“I think it’s inevitable for the vaccines to maintain tip-top efficacy, they will need to be updated. The only question is how often and when,” says Paul Bieniasz, a virologist at the Rockefeller University in New York City who co-led one of the neutralizing-antibody studies.
How should we decide when to update vaccines?
Scientists, health officials and vaccine makers are starting to hash this out. Researchers are only beginning to learn how different mutations alter vaccine responses and how evolutionary forces can cause mutations to spread. “I certainly wouldn’t update them now,” says Bieniasz.
One model that COVID-19 vaccine updates could follow is that of seasonal flu vaccines, says Subbarao, who directs the World Health Organization Collaborating Centre for Reference and Research on Influenza in Melbourne. Centres, including hers, monitor emerging flu strains for genetic changes that might influence vaccines’ effectiveness. Researchers use studies with ferret and human antibodies to determine whether a new flu strain is likely to evade a previous season’s vaccine, and therefore necessitate an update. These reviews are conducted annually for each hemisphere’s flu season, and changes are made only when a vaccine-evading strain is widespread, says Subbarao. “If it’s localized to one region, one country, we wouldn’t change the vaccine for the whole hemisphere.”
Generally, the threshold for updating flu vaccines is similar in magnitude to the threshold for changes in neutralizing-antibody responses that researchers have linked to the 501Y.V2 variant. But it is not yet clear how these shifts — and the geographical distribution of different variants and mutations — will inform COVID-19 vaccine updates. “Those discussions are just beginning,” says Subbarao. “We can’t be chasing every variant that emerges.”
How will the vaccines be updated?
That’s another open question. Some COVID-19 vaccines, including the major ones made by Moderna, Pfizer and AstraZeneca, instruct cells to produce the virus’s spike protein — the immune system’s key target for coronaviruses. Variants including 501Y.V2 carry spike mutations that alter regions targeted by neutralizing antibodies.
One possibility is to swap vaccines’ old versions of the spike protein — based largely on the virus that was first identified in Wuhan, China — for an updated molecule that has the specific amino-acid changes that hinder antibody responses. But researchers will first need to determine whether any such changes have knock-on effects that alter how the immune system reacts to the vaccine. Another possibility is to include both new and old forms of the spike protein in a single jab — scientists call this a multivalent vaccine.
Moderna has started work on updating its mRNA vaccine to match spike mutations in 501Y.V2. The biotech company, based in Cambridge, Massachusetts, says it also intends to test the effectiveness of a third dose of its original coronavirus vaccine, and is looking into the possibility of a multivalent vaccine, said Tal Zaks, Moderna’s chief scientific officer, in a 25 January call with investors. But before deciding on any path, researchers will need to study how animals, and probably humans, respond to any potential vaccine update, says Subbarao.“It’s not going to be as simple as [altering] an amino acid site and saying ‘okay we got it’.”
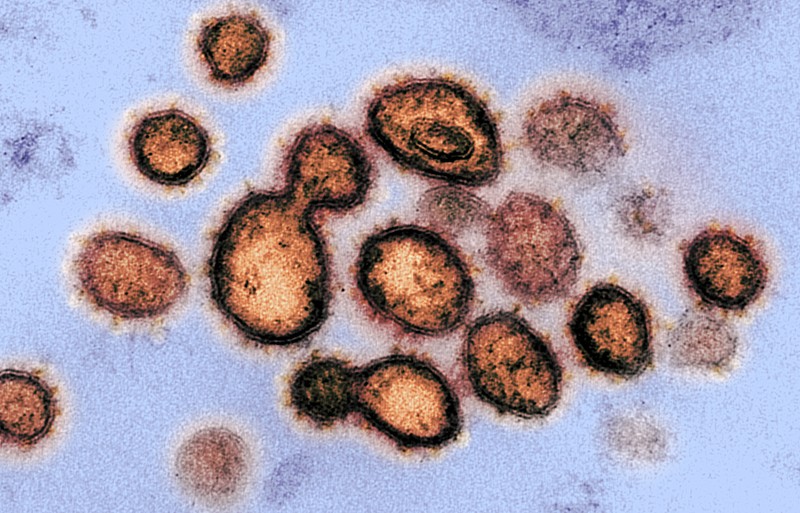
The SARS-CoV-2 virus has acquired several mutations that are changing its behaviour.Credit: NIAID-RML/NIH/Flickr
How will vaccines be trialled and approved?
Vaccine developers tested the currently available COVID-19 vaccines in phase III trials involving tens of thousands of participants before regulators authorized the drugs' use. But that kind of testing for a revamped vaccine would be slow and difficult now that the first-generation vaccines are being deployed worldwide, says immunologist Drew Weissman at the University of Pennsylvania in Philadelphia: “I can’t imagine how they could do a phase III trial for a variant.”
It’s unclear how much clinical data would be needed to approve a COVID-19 vaccine update. New seasonal flu vaccines typically do not require fresh trials. But regulators do not have the assurance of decades of experience and clinical data with COVID-19 vaccines. “They might say, ‛It’s a brand new vaccine, let’s do a couple of clinical trials,’” says Weissman.
The size and duration of those trials could depend on whether researchers can find ‛correlates of protection’: measurable features of an immune response, such as a particular level of neutralizing antibodies, that can provide a marker for protection against COVID-19. With such markers, researchers would not need to wait for trial participants to become infected with coronavirus to know whether the vaccines are working — they could simply measure immune responses after each dose.
There is no guarantee that a robust correlate will emerge, says Paul Offit, a vaccine researcher at the Children’s Hospital of Philadelphia in Pennsylvania. But even without a definitive correlate, researchers might still be able to demonstrate that their new vaccine produces antibody levels similar to the first-generation vaccines. Moderna has said that it expects to be able to rely on clinical trials involving hundreds, rather than thousands, of participants to push forward with its vaccine against the 501Y.V2 variant. Foroohar expects that it will take the company about five months to go from producing the new vaccine to submitting data from its trials to regulators.
How will people respond to updated vaccines if they’ve already been immunized?
Researchers don’t yet know how a person who has been fully vaccinated with a first-generation COVID-19 vaccine will respond to a fresh vaccine against a new variant. Immunologists have long observed that people tend to mount more robust immune responses to the first variant of a pathogen that they encounter than subsequent variants. This phenomenon could mean that updated vaccines might trigger more muted immune responses than those to a first vaccine. “The fear is that boosting somebody with a variant won’t make a new response against that variant,” says Weissman. “It’ll just boost the old response.”
But Weissman argues that there is some evidence that RNA vaccines may not fall prey to this trend. For reasons that are not clear, some RNA vaccines trigger surprisingly complex immune responses, yielding antibodies that target regions of viral proteins that are often not detected in responses to other kinds of vaccines. This could mean that RNA vaccines will also be better able to target the changes present in a variant, Weissman says.
And Offit notes that a variant-specific response may not be necessary: even if an updated vaccine mainly boosts the response to an earlier coronavirus vaccine, that may still be enough to fend off the variants, he says.
What are vaccine makers doing?
Like Moderna, other coronavirus vaccine makers have said that they are looking into updating their vaccines. They include Johnson & Johnson of New Brunswick, New Jersey, which is developing a single-shot coronavirus vaccine.
Some aspiring vaccine makers have had their eye on the threat that escape variants might pose from the start. A team at Gritstone Oncology decided to focus on this potential problem by designing a vaccine that targets multiple sites on several viral proteins, in contrast to first-generation shots that target only the spike protein, says Andrew Allen, president of the company in Emeryville, California. The hope is that the vaccine, which should soon start clinical trials, will make it difficult for the virus to evade immunity because many genetic changes would be necessary for it to do so. “You can either play whack-a-mole and chase the variants, or you can try to get ahead of them,” Allen says.
Because updating the construction of exisiting vaccines is relatively simple, a new RNA vaccine could be designed and manufactured for clinical testing within six weeks, Weissman estimates.
But that is only the beginning. “Mass-producing a vaccine is hard. To start all over again will be hard,” says Offit.
Some researchers are expecting periodic updates to coronavirus vaccines, as with flu, to become a way of life. “This is not unusual,” says Stanley Plotkin, a consultant who advises companies on vaccines. But it could mean that worries over supply chains and logistics will continue for some time.
No comments:
Post a Comment