Maj. Victoria Fernandes Sullivan, MD, U.S. Army
Strong reasons make strong actions.
—William Shakespeare, The Life and Death of King John
 On 31 December 2019, China reported the first cluster of cases of COVID-19 to the World Health Organization.1 Less than one month later, the first case arrived in the United States, and within the next two months, the deadly virus had spread across the entire country. On 28 March 2020, the first U.S. service member died; he was Army Capt. Douglas Linn Hickok, a physician assistant.2 As of this publication, the death toll in the United States is over 180,000 and continues to rise.
On 31 December 2019, China reported the first cluster of cases of COVID-19 to the World Health Organization.1 Less than one month later, the first case arrived in the United States, and within the next two months, the deadly virus had spread across the entire country. On 28 March 2020, the first U.S. service member died; he was Army Capt. Douglas Linn Hickok, a physician assistant.2 As of this publication, the death toll in the United States is over 180,000 and continues to rise.It is not too late for the United States to avoid hundreds of thousands of deaths. The crisis can be controlled by strong, competent, military medical leaders who are accustomed to practicing in resource-constrained environments (and who focus on patient triage to do the most good for the most people). This crisis must be fought by all who are integral members of the medical team and led by physicians and researchers who are subject-matter experts in clinical medicine and leadership.
The U.S. health care system has struggled to learn about COVID-19 and the sickness it causes. The civilian health care system is a patchwork of public and private clinics and hospitals. Raquel Bono, director for COVID-19 Health System Response Management, led an effort to coordinate the virus response in Washington state.3 She is a surgeon trained in general surgery, trauma, and critical care and is exceptionally qualified to lead the effort. However, there are infectious disease specialists, disaster medicine doctors, and scientists who may have more subject-matter expertise regarding COVID-19 and pandemics in general. Why was Bono selected? Her selection was almost certainly due to her leadership experience. Bono is a retired Navy vice admiral and is the former director of the Defense Health Agency. She served in numerous leadership positions throughout her military career, including during Operations Desert Shield and Desert Storm, and this experience sets her apart from other doctors. In times of crisis and operations within complex environments, subject-matter experts are not enough; leaders are needed.
Another group of military physician-leaders anticipated the challenges of the pandemic and realized that clinicians who normally do not take care of critically ill patients would be expected to do so in many military facilities. Within a matter of weeks, critical care doctors Lt. Col. Renee I. Matos and Col. Kevin K. Chung led a multidisciplinary team of fifty-five personnel in developing and publishing the Department of Defense’s COVID-19 Practice Management Guide. It is a concise document of information that clinicians need to know in order to care for patients critically ill with COVID-19.4
In times of crisis and operations within complex environments, subject-matter experts are not enough; leaders are needed.
All over the country, U.S. military physicians and scientists are leading efforts to respond to the COVID-19 pandemic. In a memorandum to Department of Defense (DOD) personnel, Secretary of Defense Mark Esper wrote that military medicine is critical to the Army’s “whole-of-nation response to the coronavirus,” from providing civilian hospitals with medical supplies to deploying the Navy’s two hospital ships and multiple Army field hospitals. He concludes by writing, “Our world-class doctors and scientists remain on the leading edge of vaccine and treatment development.”5
The current COVID-19 pandemic is proving a point that physicians and scientists who are well-trained and practiced in the art of leadership are needed to ensure the U.S. Military Health System (MHS) is able to protect and save service members in times of chaos such as pandemics and large-scale combat operations.
Past Contributions of Military Medicine
During the Civil War, two-thirds of Union and Confederate soldiers died of illnesses such as pneumonia, typhoid, dysentery, and malaria rather than from injuries on the battlefield.6 With medical professionals including medics, nurses, physical and occupational therapists, veterinarians, dentists, and doctors joining the ranks, soldiers had a better chance of surviving diseases and wounds. The achievements of military medicine have also profoundly changed modern civilian medicine; breakthroughs in triage, treatment of traumatic brain injuries and posttraumatic stress disorder, artificial limbs, and blood transfusions are just a few examples.7 Military physicians and scientists lead in innovation, research, and development.
Medical Threats in Today’s Operational Environment
Even with these medical advancements, the Army faces daunting current and future medical threats; the COVID-19 pandemic is proof. The U.S. military saw the effects the 1918 influenza pandemic had on its combat power.8 Other naturally occurring threats such as malaria, the Zika virus, and Ebola have presented challenges to our country as well. Weaponized chemical, biological, radiological, and nuclear capabilities are no longer limited to the arsenals of superpowers. Conventional forces across the world are racing to develop more lethal weapons. The space and cyber domains are now contested, presenting a threat that medical operations could be shut down in seconds. In large-scale ground combat operations, there is a likelihood that supply chains will be disrupted and units will be isolated, which will require medical personnel to provide prolonged field care in austere, resource-constrained environments. Civilian doctors will likely need to be drafted.
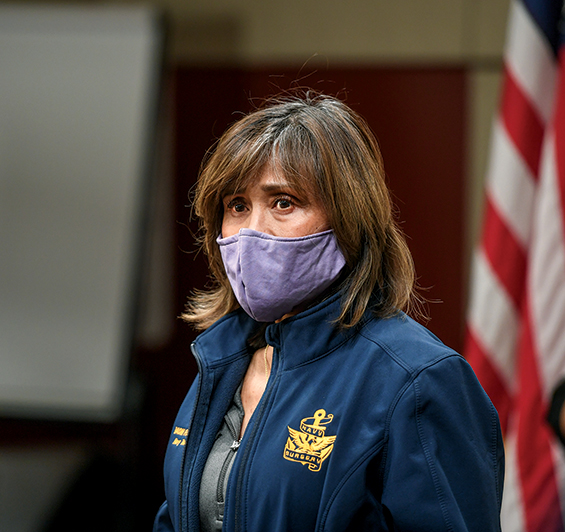
The Washington state director for COVID-19 Health System Response Management, retired U.S. Navy Vice Adm. Raquel Bono, holds a press conference 10 April 2020 at the Spokane City Fire Training Center in Spokane, Washington. (Photo used with permission by Dan Pelle, The Spokesman Review)
Today’s hurdles such as too few ventilators and medical staff to treat the high volume of patients foreshadow some of the medical challenges the United States will face in large-scale ground combat operations.
The U.S. military is a learning organization and has responded to past, present, and anticipated medical threats by prioritizing research, education, and development in the medical field. The U.S. Army Institute of Surgical Research, the Armed Forces Institute of Regenerative Medicine, Walter Reed Army Institute of Research, and the Army’s Telemedicine and Advanced Technology Research Center are dedicated to medical missions that will protect soldiers from myriad threats and improve survival rates of the wounded.9
These organizations are critically important to driving medical innovation and anticipating medical threats. However, their budgets are insufficient. The organizations’ funding has been threatened in the past and may be in the future. Having leaders at their helms who are scientists and physicians that understand the work and can articulate how it contributes directly to the strength of the U.S. military and to the United States is crucial. Research and development are only as useful as the end users, which in this case is the MHS.
Changes to the Military Health System
The MHS’s mission is to ensure the health of service members; ensure all medical personnel are trained and ready to support the operational force; and provide a medical benefit to service members, retirees, and their families.10 The MHS has operated in an environment of uncertainty for the past three years because of a number of changes. Medical facilities are undergoing reorganization under one common chain of command, the Defense Health Agency, rather than under each military branch. The Pentagon planned to cut nearly eighteen thousand medical billets to reshape the force, though those plans are now on hold.11 Some hospitals and clinics are either closing or are no longer serving retirees and dependents. The system by which Army doctors and nurses are deployed has changed. Finally, the electronic health record is being replaced. The EMR previously consisted of at least four legacy systems. In an effort to improve coordination and data sharing between the military and veterans’ health care systems, a commercial-off-the-shelf system called MHS Genesis is replacing those legacy systems. It is being fielded throughout the MHS in waves, starting in September 2019, with completion expected by 2024.12
The future vision of military medicine is in question. The National Defense Authorization Act for Fiscal Year 2017 called for a complete reorganization of military medicine to minimize redundancies between services offered by the Army, Air Force, and Navy health systems. To lead this change, the Defense Health Agency was created and charged with the administration of every military medical treatment facility; this transition is happening now.13 The transition may mean fewer leadership positions are available to military doctors at medical treatment facilities because these positions can be filled by civilians.
Another change for the Army Medical Corps (MC) in 2019 was that the professional filler system was replaced by the modified table of organization and equipment assigned personnel system.14 With the professional filler system, Army physicians were assigned to hospitals or clinics and would be attached to a unit for a deployment. Now, under the modified table of organization and equipment assigned personnel system, physicians and other health care personnel are organic to a unit but report to a military hospital or clinic for work every day. Their chain of command can recall them to the unit as needed for training, administrative tasks, and deployments. One potential implication of this change is it will be more difficult for doctors to receive “top-block” ratings on officer evaluation reports since they must balance their duty requirements with their unit as well as with the hospital.
Identifying the Leadership Gap in the Army Medical Corps
Amidst all of the changes listed above, physicians continue to provide excellent patient care throughout the DOD. Within the next few years, the effects these changes will have on the military will be visible. The medical corps must be involved at every level to ensure that the changes do not negatively impact patients. The MC must also advocate for physicians and all personnel at the bedside who are critical to the health care team. Herein lies a gap in the MC; more doctors must be formally trained in leadership to help the MHS navigate uncertain waters, including this pandemic, and the threat of large-scale ground combat operations.
The military excels at leadership. Leadership is developed through on-the-job training and mentorship. Many officers will pursue graduate degree programs, often in subjects that emphasize leadership, such as a master’s in business administration (MBA) or a master’s in leadership. In fact, the Army has broadening opportunity programs, the intent of which is “to develop an officer’s capability to see, work, learn, and contribute outside each one’s own perspective or individual level of understanding for the betterment of both the individual officer and the institution. The result of broadening is a continuum of leadership capability at direct, operational, and strategic levels.”15
Unfortunately for physicians and scientists with doctoral-level degrees, these broadening leadership opportunities are unavailable, yet physicians need these skills as well. Many medical schools do not include consistent, formalized leadership instruction in their curriculum. Currently, if a physician wants to develop his or her leadership skills, it will likely be on his or her own time and with his or her own dime. For example, the handful of military physicians who have an MBA, a master’s in health administration (MHA), or a similar degree have either paid out of pocket to do coursework online (a significant time burden on them and their families), or in a few cases, took two years off from practicing medicine to obtain their MHA/MBA degree through the Army-Baylor University program.16
There are senior-level physicians who are passionate about leadership, but the MC should not depend on the Herculean efforts of these few to teach leadership.17 The Army’s current approach to developing physicians as leaders places the onus on the individual and his or her family rather than incentivizing the development and taking the pressure off of the physicians. Here lies an enormous opportunity for the Army to develop its physicians as officers, improve physician retention, and increase employee satisfaction in the MC by showing that the organization values its physicians. From a strictly utilitarian standpoint, adding depth to the pool of formally trained military physician-leaders will help ensure medical performance is optimized during times of crisis, such as pandemics and during large-scale ground combat operations.
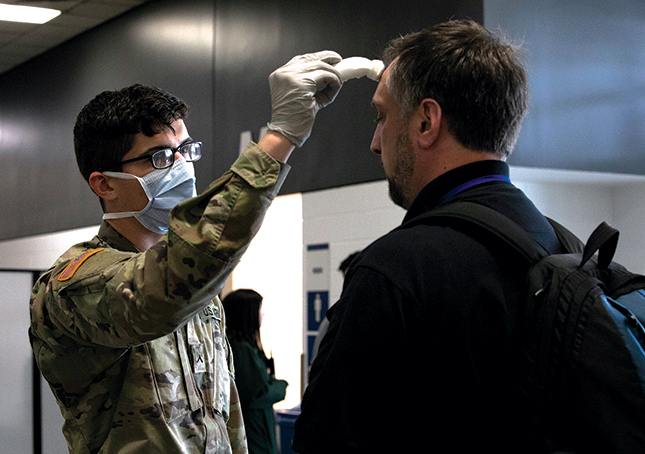
A soldier checks the temperature of a civilian 5 April 2020 at Century Link Field Event Center in Seattle. Approximately five hundred soldiers from Joint Base Lewis-McChord, Washington, and Fort Carson, Colorado, assembled and operated an Army field hospital in support of the COVID-19 response. (Photo by Pvt. 1st Class Genesis Miranda, U.S. Army)
Closing the Gap
How can the Army operationalize better leadership training for its physicians? Almost one decade ago, leaders in the MC published “All Physicians Lead,” a document that sought to improve leadership training in the MC.18 However, to my knowledge, none of their recommendations have been implemented corps-wide.
To a corps engrossed in taking care of patients, training the next generation of doctors, and deploying, adding more mandatory training will be detrimental. Leadership training should be voluntary but encouraged and supported. The following approach may be practical for busy professionals:
Adopt a formalized leadership curriculum to be used either in graduate medical education or once doctors have completed training. This curriculum should include didactics on conflict management, emotional intelligence, self-awareness, decision-making skills, and influence. Many organizations have developed rigorous leadership curricula before now, so any new curriculum does not need to be developed from scratch; however, military-specific lessons must be added to any preexisting curriculum (e.g., “All Physicians Lead,” “Lead 2.0” curriculum).
Continue to develop leadership skills in the workplace. Once a foundation of knowledge has been gained, students of leadership must develop these skills. Much of this can happen through working in their usual jobs and leading medical teams. Additional leadership development opportunities should not be cumbersome; they can be combined with professional development. Doctors can be sent to medical conferences where networking occurs and leadership sessions are offered. Leadership retreats during the work week are another avenue to deliver this development opportunity without infringing on precious free time and family time. Mentorship allows leaders to continue to develop, and this is an area in which the military excels.
Finally, provide a pathway for those who want to be operational and strategic leaders. Currently, master’s degrees such as MBAs are not supported for those with doctoral-level degrees. Remove this hurdle. Having a doctorate in medicine should not preclude an officer from developing themselves further in another subject as long as these skills will serve the military and the individual. Preserve the opportunity for physicians to attend the Command and General Staff College in residence. The leadership curriculum offered at the Command and General Staff College is invaluable, as is the opportunity to work with and learn from peers from other branches, services, and nations. This experience is not replicated at satellite schools or in distance learning. Work with Baylor University to create a flexible MHA/MBA curriculum that allows physicians to attend the program while continuing to care for patients at the bedside. One oft-named barrier to pursuing formal leadership training is that physicians do not want to lose their clinical skills or take time away from caring for patients to attend school. If the curriculum was amended so that doctors could attend class and still care for patients, more of the MC may compete for the Baylor MHA/MBA program.
Some say the majority of physician billets in the military can be adapted for civilians or that physicians within the military can be limited to clinical roles and excluded from leadership roles. However, if these changes happen, there will be a dearth of leadership skills among physicians during crises and deployments. The evidence is growing that good leadership “positively influences both patient and healthcare organization outcomes.”19 A 2016 Harvard Business Review article summarized multiple studies that support the premise in which physicians are good hospital leaders for a variety of reasons: they are domain experts, they are dedicated to patient care, and they have peer-to-peer credibility.20
Many civilian doctors are not trained in leadership and do not have experience with it. Few medical schools include consistent, formalized leadership didactics in their curriculum. A systematic review of leadership training in graduate medical education reviewed over three thousand publications in medical literature and found that the leadership curricula that do exist in medical schools are “heterogeneous and limited in effectiveness.”21
What We Ought to Be
Change is difficult in a large organization such as the U.S. military, and yet it is not impossible, as more than a century of medical innovation and leadership shows. Officer physicians must steward the profession and lead the MHS through change and challenges and emerge stronger from each one. Gen. Douglas MacArthur seems to have been speaking directly to Americans during these trying times when he said,
Duty, Honor, Country: Those three hallowed words reverently dictate what you ought to be, what you can be, what you will be. They are your rallying point to build courage when courage seems to fail, to regain faith when there seems to be little cause for faith, to create hope when hope becomes forlorn.22
Fellow physicians, scientists, clinicians, and military leaders, in this forlorn moment of human history, we must rally with courage, faith, and hope, and strive to be what we ought to be and can be.
No comments:
Post a Comment