By Ursula Jasper for Center for Security Studies (CSS)
 Due to global mobility and the deeply interconnected nature of the contemporary world, national efforts do not suffice to keep infectious disease such as Ebola, SARS or H1N1 from spreading across borders. As a result, states must coordinate their efforts to identify and contain outbreaks as quickly as possible. To that aim, Ursula Jaspers contends, the international community must do more to improve the implementation of the WHO’s International Health Regulations.
Due to global mobility and the deeply interconnected nature of the contemporary world, national efforts do not suffice to keep infectious disease such as Ebola, SARS or H1N1 from spreading across borders. As a result, states must coordinate their efforts to identify and contain outbreaks as quickly as possible. To that aim, Ursula Jaspers contends, the international community must do more to improve the implementation of the WHO’s International Health Regulations.
Protection from infectious diseases has become a key issue not only in Swiss, but also in international health policy in recent years. Under the terms of the WHO’s International Health Regulations (IHR), which are at the center of these efforts, states must identify and contain outbreaks at the earliest possible stage. However, the global implementation of the regulations must be further improved.
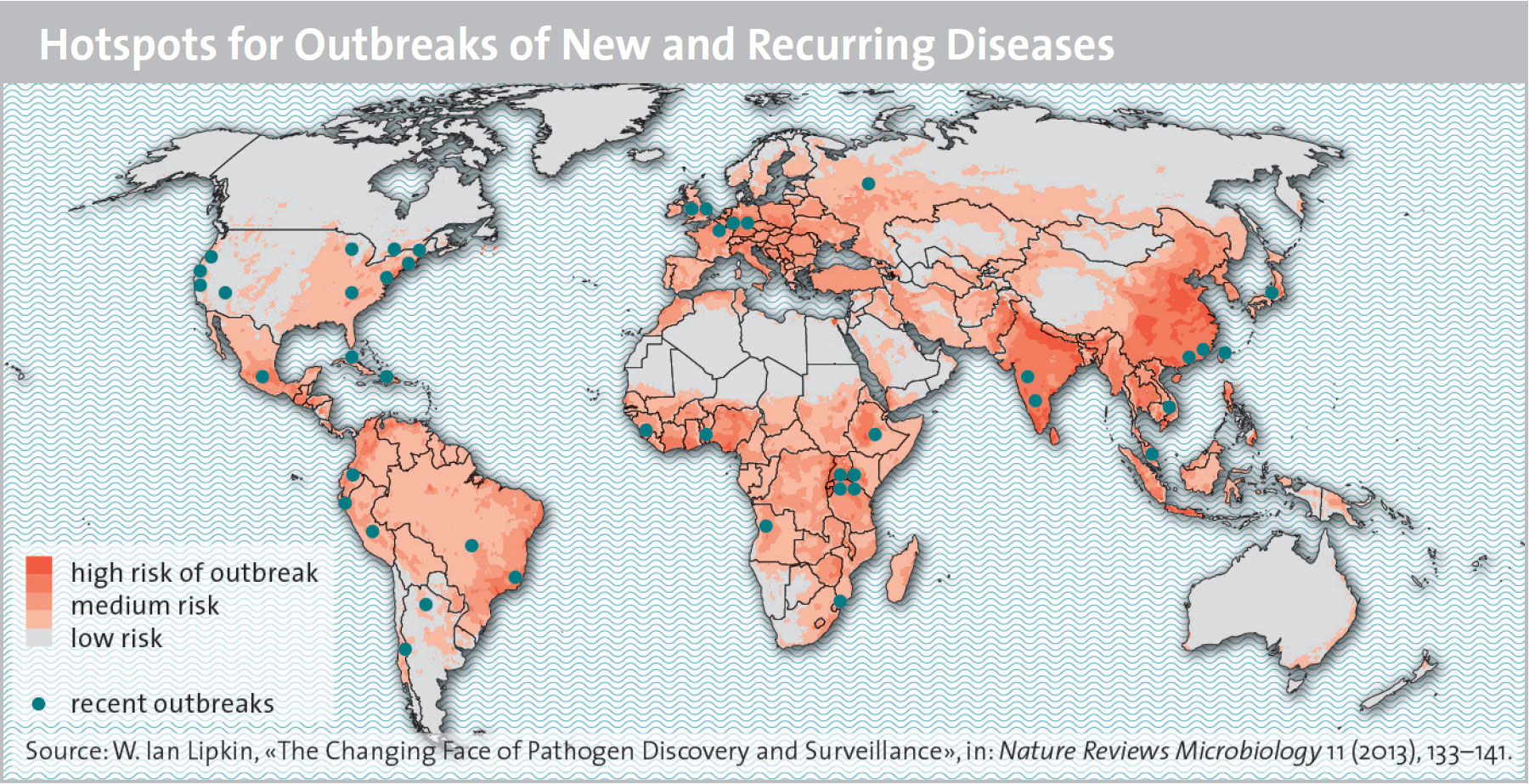
SARS, MERS, H1N1, Ebola, Zika – the list of infectious diseases that have alarmed the public and challenged researchers around the globe in recent years is a long one. Today more than ever, communicable diseases are regarded as serious potential threats to national and global society. For instance, the WHO in 2007 described the danger of a new type of influenza virus as “the most feared security threat” (World Health Report 2007, p. 45). Health experts warn that increasing global mobility as well as interdependencies and interconnections due to flows of trade and goods, migration, and tourism create the conditions for a spread of global, i.e. pandemic diseases within a short time. This means that purely national efforts to combat diseases are ineffective, and that transnational, joint approaches are necessary.
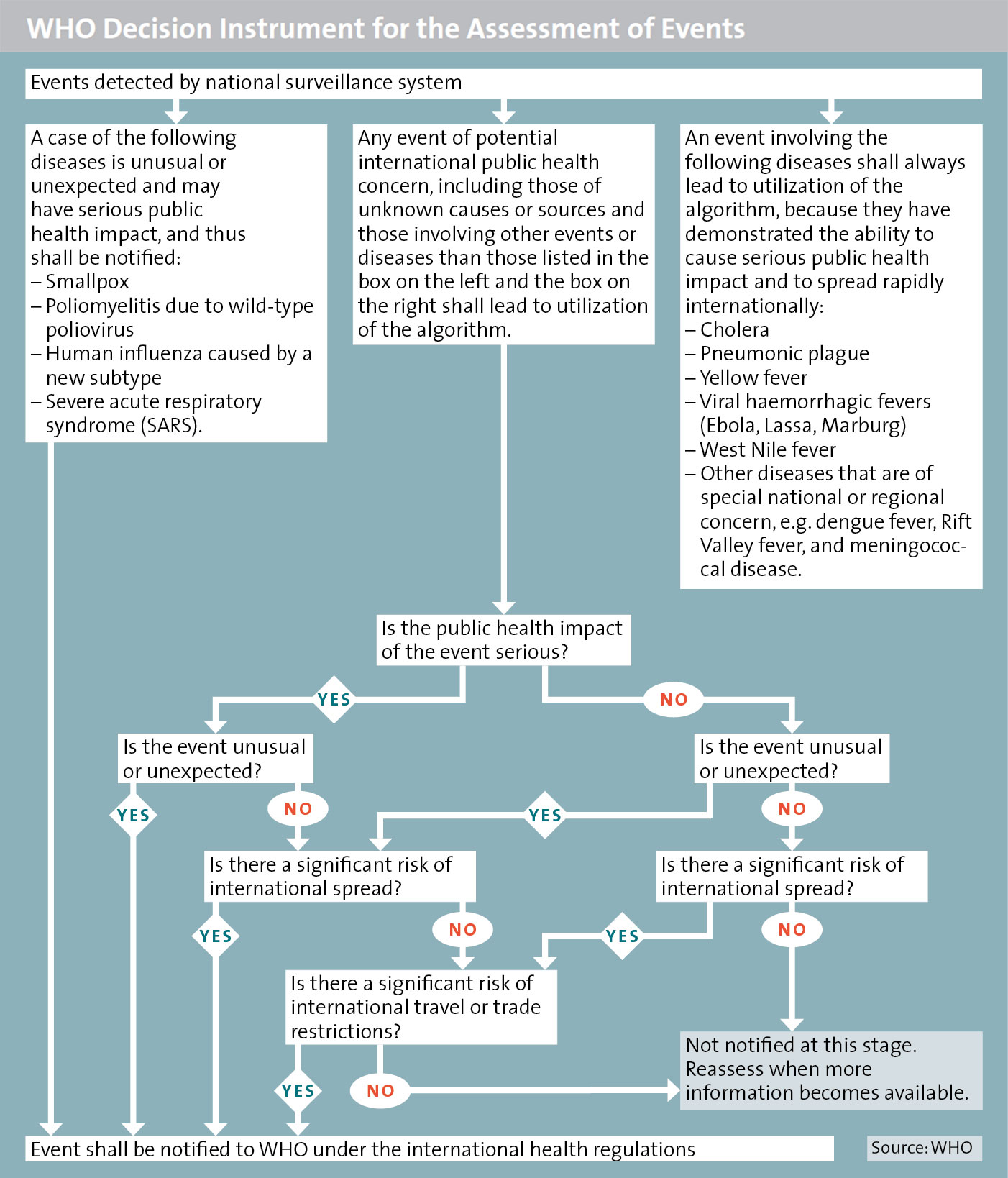
Therefore, after years of negotiations, the WHO passed a new set of International Health Regulations (IHR) in 2005. They stipulate that all WHO member states must build up national early detection and warning systems to be able to discover and respond in a timely manner to potential cross-border pandemics – known as Public Health Emergencies of International Concern – on their territories.

The Zika virus transmitted by mosquitoes in 2016 has led to a “Public Health Emergency of International Concern”. Paolo Withaker / Reuters
Historic Roots
International efforts at protection against communicable diseases are by no means a new phenomenon. Already in the 14th century, city-states like the Republic of Venice imposed quarantine regulations on traders and travelers – usually unilaterally – to protect themselves against the introduction of pathogens such as the plague. Ships’ crews had to lie at anchor off the coast for 40 days (in Italian: quarantina di giorni) before they could go ashore and unload their cargo.
However, the earliest instance of what one might call true inter-state cooperation began in the year 1851, when 12 states met in Paris for the first International Sanitary Conference. Its purpose was to harmonize international rules for dealing with communicable diseases, especially cholera, and to elaborate a set of mandatory regulations. The conference, as well as roughly a dozen follow-up conferences, discussed ideas on how states could protect themselves from the spread of diseases without jeopardizing the free exchange of goods and people. The conferences laid the groundwork for an international health regime that would remain in force over the following decades and was guided by two main principles: On the one hand, participating states agreed to exchange information about outbreaks of certain diseases within their borders. On the other hand, they vowed to ensure that measures to ward off health threats and protect against the spread of diseases would not unduly affect cross-border trade. Regulations and restrictions were to be in line with the accepted scientific standards of the day. The foundation of the WHO in 1948 helped to harmonize various regional approaches and treaties and to create an internationally recognized coordinating body. Especially in the first decades of its existence, this Geneva-based organization focused mainly on the fight against infectious diseases. Among its primary responsibilities are coordination work in the technical and bioscience fields, the formulation of medical standards, and the systematic collection and publication of information about outbreaks (also known as epidemic intelligence).
The 1990s: Impetus for Reform
Despite the organization’s successes, for instance in eradicating smallpox in the 1970s, the global regime for combating communicable diseases has been severely flawed. For instance, countries have often covered up outbreaks of diseases on their territory due to concerns over negative economic effects and reputational damage. Moreover, the mandatory information exchange had been limited to just a handful of diseases: While the initial list had consisted of six reportable diseases (cholera, plague, yellow fever, smallpox, typhoid, and relapsing fever), by 1995 that list had been reduced to just three (cholera, plague, and yellow fever). After a number of severe outbreaks in the 1990s, including a cholera epidemic in South America and an Ebola epidemic in what was then Zaire, the WHO decided in 1995 to revise the regulations on disease control.
However, it was not until the SARS outbreak of 2002/2003 that the topic gained sufficient urgency to prompt an agreement. The emergent disease, caused by a hitherto unknown virus, spread globally within weeks, stoking fears of an uncontrollable “killer virus”: A patient from China’s Guangdong province had travelled to Hong Kong for a wedding, where he infected other guests, who in turn transmitted the infection as they continued on their journeys. In this way, the virus managed to spread swiftly along international high-frequency travel routes to Singapore, Vietnam, and Canada. Within a few months, more than 8’000 people in 25 countries on five continents had fallen ill, and 800 had died.
‘New’ Rules
Against the background of the SARS pandemic, the WHO member states agreed in 2005 to implement a far-reaching reform of applicable health regulations. On the one hand, all regulations were still designed to facilitate a balance between measures to control and contain infectious diseases and the need to minimize their impact on the cross-border movement of goods and people. However, WHO member states are now subject to much more comprehensive requirements, three of which are especially important: the expanded reporting scheme, the obligation for members to create national reporting systems and capacities for protection measures, and the involvement of non-state actors.
First of all, it is important to note that the most radical change in regulations relates to reportable disease outbreaks. Unlike in earlier years, today states must report not only outbreaks of specific diseases from a predetermined list, but also any events that pose a threat to public health and might constitute a “Public Health Emergency of International Concern”. These may include both known diseases such as cholera, yellow fever, or Ebola and novel, hitherto unknown diseases, irrespective of their cause or provenance. States party to the treaty are obliged to base their evaluation of events on a decision instrument (cf. box above). The decisive factor is not the cause of the disease, but its degree of severity and the danger of a cross-border spread. This is to ensure that events that cannot be attributed to a known pathogen or any apparent cause will also be reported. Such causes may include not only new, hitherto unknown pathogens (cf. box below), but in theory also outbreaks resulting from biological or chemical agents or radiological material.
Secondly, the WHO member states are committed to building up comprehensive capacities across their entire territory for identifying, reporting, and combating disease outbreaks in order to be able to record relevant events quickly and report them to the WHO within 24 hours of discovery. To this end, each state must designate a national IHR focal point (in Switzerland, this is the Federal Office of Public Health) that remains in permanent contact with the WHO and is responsible, in the case of an event, for internal and external communication between the WHO and authorities on the ground. Additionally, states must establish a functioning reporting system at all administrative levels (municipal, intermediary, and national) within five years if none is already in place. This means, for instance, ensuring that information such as clinical descriptions of the outbreak, laboratory results, the numbers of patients and casualties, and public health measures is gathered at the local level before being passed on to the next higher level of authority, and that first response measures can be taken immediately. Moreover, the regulations require states to elaborate national response plans for health crises and to create logistical capacities and multi-disciplinary task forces that can implement measures on the ground at any time.
Thirdly, under the new health regulations, the WHO no longer depends exclusively on the cooperation and reports of national governments. It may now also declare a public health emergencies of international concern and recommend measures based on information from non-state actors – if necessary, even without the consent of the affected state. This is especially important given recent developments in telecommunications technology: A large number of internet-based information media in the field of digital disease surveillance are engaged today in gathering epidemiological information about potential outbreaks and unusual medical conditions.
National and Global Implementation
In Switzerland, the Federal Council approved the IHR in 2006 and authorized adaptations of relevant passages in national legislation. Since the country already had in place many of the required capabilities in the field of disease monitoring and control, independently of developments at the WHO, the significant changes in Switzerland mainly involved a revision of the Law on Epidemics and adjustments of national and cantonal pandemic plans. Particular attention was devoted to delimiting and streamlining jurisdictions between the cantons and the federal administration in crisis situations. Bundling responsibilities and ensuring coherent crisis management within the country’s federal system proved to be the main challenge. One major innovation is a three-level escalation model for normal, particular, and extraordinary conditions, under which authority is progressively shifted towards the federal level depending on the gravity of the situation. Federal and cantonal pandemic plans also lay out the concrete strategic response to a pandemic event, including the logistics of vaccine and medicine distribution and of medical care, as well as general principles of conduct and communication.
However, for other states, the adoption of those regulations into national legislation, and in particular the provision of the necessary medical and logistical infrastructure, poses greater problems: As of the end of 2016, less than 75 per cent of countries around the world had implemented the IHR and created the required core capabilities. Especially for developing countries, many of which have only rudimentary healthcare systems and very limited funds to spend on them, complying with IHR requirements is a major challenge. Also, critics fear that states might find themselves forced to reallocate resources within the healthcare system. In such a case, creating the required capabilities might come at the expense of basic healthcare or other priorities, such as reducing infant mortality. Without concrete international financial aid, which was originally not envisaged, it will therefore be difficult to achieve the IHR’s standards globally without jeopardizing other health goals.
Furthermore, many critics point out that the new IHR mainly reflect the priorities of the industrialized nations, and that their main purpose is to allow rapid detection of communicable disease outbreaks in the south to prevent them from spreading to the north. In order to contribute at a fundamental level to global health security, these critics argue, efforts would have to also address the causes of diseases, such as poverty, lack of hygiene, insufficient basic medical healthcare, or lack of access to medication.
One of Many Building Blocks
The dramatic and long-ignored spread of the Ebola epidemic in West Africa in 2014, nearly a decade after the adoption of the IHR, has indeed raised questions over the new health rules and their contribution to global health security. More than 30’000 people fell ill in the most afflicted states of Sierra Leone, Liberia, and Guinea alone, with 11’000 people dying from the epidemic. The WHO was criticized for having responded to the outbreak too late and too hesitantly: It was not until four-and-a-half months after the disease had erupted, and two-and-a-half months after Médecins Sans Frontières had described the situation as “out of control”, that the Geneva-based organization proclaimed an international public health emergency.
At the same time, the outbreak illustrated that the global regime for defense against infectious diseases is only as strong as its weakest link, which is local healthcare. States must have at least a minimal functioning healthcare infrastructure in order even to be able to implement and operationalize the IHR. That requires both financial and technical support by the WHO and the industrialized countries. The progressive fragmentation of the global health architecture over many years has not been especially helpful in this context: Private and public initiatives, trusts and NGOs, corporations, national health authorities, multilateral initiatives such as the G7 or G20, and international organizations such as the International Monetary Fund (IMF) or the World Trade Organization (WTO) have become influential actors in the sphere of healthcare policy, undermining the coordination and leadership role of the WHO.
Furthermore, massive budget cuts have forced the organization to slash many jobs both at its headquarters in Geneva and in regional offices, leading to a loss of expertise that cannot be immediately restored in the case of an acute health crisis. In this context, Switzerland’s intention to lobby for a strengthening of the WHO and a consolidation of the global health architecture is particularly salient.
However, the Ebola outbreak also illustrates another fundamental weakness of the global health architecture: The virus that causes the disease is by no means new, and has in fact been identified since the 1970s. Nevertheless, until 2015, no vaccine was available, since under “normal” market conditions and profitability expectations, there is little incentive for the pharmaceutical industry to invest in research into diseases that are relatively rare or occur mainly in poor countries. New financing models and public-private partnerships (e.g., the World Bank’s Pandemic Emergency Financing instrument or the Global Fund to Fight AIDS, Tuberculosis and Malaria) are required to steer research and development in this direction. However, already today, observers warn of the dangers if healthcare is further “marketized” and subordinated to economic considerations.
The adoption of the International Health Regulations in 2005 can therefore only be regarded as one of many building blocks in the international health security regime. Containing the danger of pandemics efficiently will require further political, social, financial, and biotech advances in the coming years, at the national level, but especially also on a global scale.
No comments:
Post a Comment